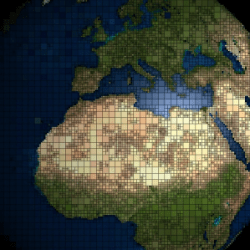
Cardiovascular diseases (CVDs) remain a staggering public health challenge worldwide. Responsible for over 17 million deaths in 2008, these diseases disproportionately affect populations in low- and middle-income countries (LMICs). As CVDs are largely preventable, this crisis calls for a robust and coordinated global response. In this comprehensive article, we explore the underlying factors, inequities, and evidence-based solutions to mitigate the impact of CVDs.
The fight against cardiovascular diseases demands urgent, sustained, and unified action. By prioritizing prevention, addressing healthcare inequities, and fostering global solidarity, we can reduce the devastating impact of CVDs. The opportunity to turn the tide on this global epidemic is within reach—and with collective effort, we can achieve a healthier, more equitable future.
Global Mortality from CVDs
CVDs account for the largest proportion of global deaths. Among these, over 3 million are premature, occurring before the age of 60. Such deaths are concentrated in LMICs, where limited access to healthcare and resources exacerbates outcomes. In stark contrast, high-income countries have witnessed significant reductions in premature mortality due to advanced healthcare systems and proactive public health policies.
Regional Disparities
- High-Income Countries (HICs): Premature deaths constitute only 4% of total CVD-related fatalities. This reflects effective interventions like smoking cessation programs, improved healthcare infrastructure, and public awareness campaigns.
- Low-Income Countries (LICs): Premature CVD deaths account for 42% of cases, underscoring disparities in access to preventative and curative measures. Many deaths could be avoided through basic healthcare improvements.
Trends in CVD Mortality
Over the past two decades, high-income countries have achieved substantial progress in reducing CVD mortality. Key factors include:
- Widespread adoption of preventive measures.
- Enhanced healthcare technologies for early diagnosis and treatment.
- Public awareness campaigns encouraging heart-healthy lifestyles.
Conversely, CVD mortality has surged in LMICs. Urbanization and economic transitions have led to lifestyle changes, including poor diets, reduced physical activity, and increased tobacco and alcohol use.
Preventability of CVDs
CVDs are preventable with both individual and population-level interventions. According to the Global Status Report on Noncommunicable Diseases (2010), preventive strategies can dramatically reduce the burden of these diseases. These include:
- Population-Wide Measures:
- Promoting healthy eating habits.
- Implementing tobacco control policies.
- Encouraging physical activity through community programs.
- Individual Healthcare Interventions:
- Routine screenings for hypertension, cholesterol, and diabetes.
- Evidence-based medication for at-risk individuals.
The Socioeconomic Burden of CVDs
CVDs exact a heavy toll on economies, particularly in LMICs where the working-age population is disproportionately affected. Premature deaths reduce productivity and strain families financially, compounding poverty cycles. Social systems face significant challenges as they attempt to address the escalating healthcare needs associated with CVDs.
“Best Buy” Interventions
The World Health Organization (WHO) emphasizes “best buy” interventions as cost-effective solutions for preventing CVDs. Examples include:
- Taxes on sugary drinks, tobacco, and alcohol to discourage consumption.
- Public campaigns to promote heart health.
- Affordable access to essential medicines for managing cardiovascular risk factors.
Challenges in Developing Countries
Public health systems in developing nations struggle to address the increasing prevalence of CVDs. Key challenges include:
- Overreliance on resource-intensive hospital care.
- Limited availability of trained primary care providers.
- Insufficient public health infrastructure for early detection.
As a result, many individuals remain undiagnosed or untreated, contributing to avoidable complications and deaths.
The Role of Primary Prevention
Primary prevention aims to address risk factors before they manifest as disease. Efforts in this area can prevent up to two-thirds of premature CVD deaths. Effective strategies include:
- Community education campaigns emphasizing diet, exercise, and smoking cessation.
- National policies promoting reduced sodium in processed foods.
Early detection through regular check-ups can significantly reduce the need for costly hospital-based treatments.
Healthcare Inequities
A significant contributor to the rising global CVD burden is inequitable access to healthcare. While developed countries have robust systems to manage and mitigate risks, LMICs face barriers such as:
- Financial constraints preventing access to medications.
- Geographic limitations restricting access to primary healthcare facilities.
Innovative solutions like telemedicine and mobile health units can help bridge these gaps.
International Awareness and Action
Global recognition of CVDs as a major health and socioeconomic challenge has grown. In 2011, the United Nations General Assembly convened a High-Level Meeting to address the prevention and control of noncommunicable diseases (NCDs), including CVDs. This marked a turning point in prioritizing CVD prevention within international health agendas.
The Role of the United Nations
The 2011 meeting emphasized the need for actionable strategies to combat CVDs. Participating nations committed to:
- Developing national action plans.
- Establishing measurable targets for reducing premature deaths.
- Promoting multisectoral partnerships to ensure sustainable interventions.
Surveillance and Monitoring
Accurate data is essential for effective CVD management. Surveillance systems help track:
- Prevalence of risk factors like smoking and obesity.
- Effectiveness of implemented policies.
- Progress toward reducing mortality and morbidity rates.
National-Level Strategies
Countries must adopt comprehensive approaches to combat CVDs. Key actions include:
- Strengthening primary healthcare systems to improve access.
- Implementing policies that integrate health considerations across all sectors.
- Investing in training healthcare providers to address NCDs effectively.
Global Solidarity and Collaboration
Tackling CVDs requires global partnerships that transcend national and cultural boundaries. Sharing resources, expertise, and best practices ensures equitable progress. Initiatives like the WHO’s Global Hearts program exemplify successful international collaborations.
Frequently Asked Questions (FAQs)
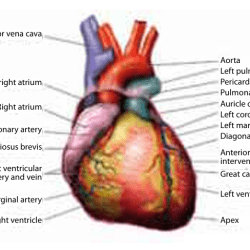
- What are cardiovascular diseases (CVDs)?
CVDs refer to a group of disorders involving the heart and blood vessels, such as coronary artery disease, stroke, and arrhythmias. - Why are CVD rates rising in low- and middle-income countries?
Urbanization, lifestyle changes, and limited healthcare access contribute to increasing rates. - What are the “best buy” interventions for CVD prevention?
Affordable and scalable measures like tobacco taxation, public health campaigns, and improved access to essential medications. - How can individuals prevent CVDs?
Maintaining a healthy diet, exercising regularly, avoiding tobacco, and monitoring blood pressure are effective strategies. - What role does the UN play in combating CVDs?
The UN fosters global collaboration, sets health targets, and supports nations in implementing policies to reduce NCDs. - How can global collaboration reduce CVD mortality?
Sharing knowledge, resources, and innovative solutions ensures equitable access to preventive and curative care worldwide.