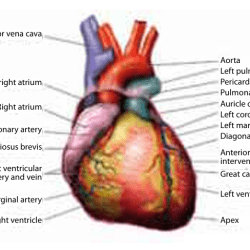
Deaths and Disabilities arising from Cardiovascular Diseases (CVDs) like Heart Attacks, Strokes
Cardiovascular diseases (CVDs), primarily heart attacks and strokes, are the leading causes of death and disability worldwide. These conditions are fueled by a combination of behavioral risk factors, including smoking, inactivity, unhealthy diets, and alcohol use. This article delves into the global burden of CVDs, the shared risk factors with other non-communicable diseases (NCDs), and the steps necessary to reduce their devastating impact.
Global Burden of CVDs
CVDs account for a staggering portion of global mortality and disability. According to the World Health Organization (WHO), 17.3 million deaths were attributed to CVDs in 2008, representing 30% of all deaths. A significant majority—over 80%—of these deaths occur in low- and middle-income countries (LMICs). Beyond mortality, CVDs contribute to 151 million disability-adjusted life years (DALYs), with coronary heart disease and stroke as the largest contributors.
Shared Risk Factors with Other NCDs
Behavioral risk factors like tobacco use, physical inactivity, unhealthy diets, and alcohol misuse are common culprits behind CVDs and other NCDs such as cancer, diabetes, and chronic respiratory diseases. Prolonged exposure to these factors leads to:
- Hypertension: A major driver of strokes and heart attacks.
- Diabetes: Damages blood vessels, increasing CVD risk.
- Dyslipidemia: High levels of abnormal blood lipids contribute to artery blockage.
- Obesity: A root cause of multiple metabolic and cardiovascular conditions.
These interconnected conditions highlight the importance of addressing shared risk factors comprehensively.
Pathophysiological Links Between Risk Factors and CVDs
CVDs often coexist with other chronic conditions. Hypertension and diabetes, for example, not only increase cardiovascular risk but also link to renal disease. Obesity exacerbates these risks by promoting high blood pressure, elevated blood sugar, and abnormal cholesterol levels. These conditions form a complex web, increasing the likelihood of heart attacks and strokes.
Epidemiological Trends in Low- and Middle-Income Countries (LMICs)
LMICs face a dual burden of communicable diseases and rapidly rising NCDs, including CVDs. Notably, the prevalence of strokes and heart attacks in these regions has doubled in recent decades, often surpassing rates in high-income countries. Compounding the issue, nearly 29% of NCD-related deaths in LMICs occur among individuals under 60, compared to just 13% in high-income countries.
Comparative Burden in High-Income Countries
High-income countries have seen declining CVD mortality due to robust healthcare systems and effective prevention programs. However, disparities persist, particularly among marginalized populations. The progress underscores the value of investment in public health initiatives and advanced medical treatments.
Disability Due to CVDs
While mortality rates highlight the severity of CVDs, their impact on disability is equally profound:
- Stroke: A leading cause of long-term disability, second only to dementia in LMICs.
- Coronary Heart Disease: Among the top five contributors to years lived with disability (YLDs) in elderly populations.
These conditions significantly reduce the quality of life for survivors, emphasizing the need for rehabilitation and support systems.
Behavioral Risk Factors and Prevention
Mitigating behavioral risk factors is pivotal in reducing CVD incidence:
- Smoking Cessation: Reduces CVD risk significantly within a few years.
- Increased Physical Activity: Strengthens cardiovascular health and lowers blood pressure.
- Healthy Diets: Diets rich in fruits, vegetables, and whole grains combat obesity and dyslipidemia.
- Alcohol Moderation: Limits its harmful effects on blood pressure and heart health.
Role of Healthcare Systems
Healthcare systems play a critical role in combating CVDs:
- Screening Programs: Early detection of hypertension, diabetes, and cholesterol abnormalities.
- Emergency Care: Timely interventions for heart attacks and strokes save lives.
- Rehabilitation Services: Support recovery and reduce the risk of recurrent events.
Economic Impact of CVDs
CVDs impose significant economic burdens, particularly in LMICs. Treatment costs, long-term care expenses, and productivity losses exacerbate financial strain, making prevention a cost-effective solution.
Population-Based Prevention Strategies
National and global campaigns addressing behavioral risk factors have demonstrated success. For example:
- Tobacco Control: Policies like increased taxation and advertising bans reduce smoking rates.
- Dietary Improvements: Public education on reducing salt and sugar intake.
- Physical Activity Promotion: Encouraging active lifestyles through urban planning and incentives.
Challenges in LMICs
Barriers such as inadequate healthcare infrastructure, limited awareness, and cultural norms hinder prevention and treatment efforts in LMICs. Addressing these challenges requires increased funding, education, and tailored interventions.
Future Projections for CVD Burden
As populations age, the global burden of CVDs is expected to rise, particularly in LMICs. Collaborative efforts between governments, healthcare providers, and international organizations are crucial to reversing these trends.
Advances in Medical Treatments and Technologies
Emerging technologies offer hope in the fight against CVDs:
- Medications: Innovations in blood pressure and cholesterol management.
- Diagnostic Tools: AI-driven systems for early detection.
- Integrated Care Models: Combining medical, behavioral, and rehabilitative services.
Call to Action
The rising burden of CVDs calls for urgent action to address behavioral risk factors, improve healthcare systems, and implement population-wide prevention strategies. Collaborative efforts are essential to saving lives and improving global health.
1. What are the primary risk factors for CVDs?
Tobacco use, physical inactivity, unhealthy diets, and harmful alcohol consumption are the main behavioral risk factors.
2. Why are CVD rates higher in LMICs?
Limited healthcare access, rising NCD risk factors, and insufficient prevention programs contribute to higher rates.
3. How can individuals reduce their risk of CVDs?
Adopting healthy habits like quitting smoking, staying active, and maintaining a balanced diet can significantly lower risk.
4. What is the economic impact of CVDs?
CVDs lead to high treatment costs, long-term care expenses, and productivity losses, especially in LMICs.
5. How does stroke compare to heart disease in terms of disability?
Stroke is the second leading cause of disability worldwide, often surpassing heart disease in terms of long-term impact.
6. Are younger populations at risk for CVDs in LMICs?
Yes, nearly 29% of NCD-related deaths in LMICs occur among individuals under 60 years of age.