Cardiovascular diseases (CVDs), including heart attacks and strokes, are the leading causes of mortality globally. Over the past two decades, high-income countries have witnessed a remarkable decline in cardiovascular mortality, thanks to advancements in prevention and treatment strategies. This article explores the primary and secondary measures that contribute to reducing the burden of CVDs.
The prevention of heart attacks and strokes requires a dual approach: population-wide initiatives and individual healthcare interventions. Together, these strategies have the potential to transform global health outcomes. Governments, healthcare providers, and individuals must collaborate to sustain and accelerate the progress achieved so far.
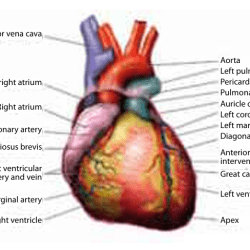
Understanding Heart Attacks and Strokes
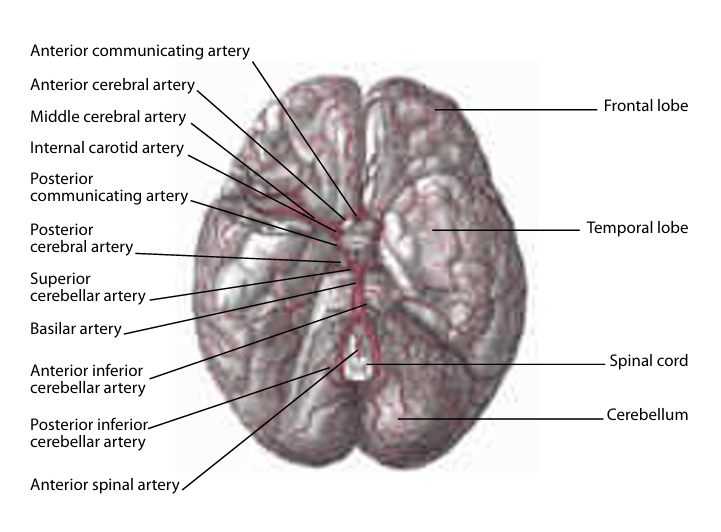
Heart attacks and strokes are severe manifestations of cardiovascular diseases. A heart attack occurs when blood flow to the heart is blocked, often due to a buildup of fatty deposits. A stroke, on the other hand, results from interrupted blood flow to the brain, caused either by a clot (ischemic stroke) or bleeding (hemorrhagic stroke).
Despite their differences, these conditions share common risk factors, such as hypertension, smoking, obesity, and a sedentary lifestyle. Understanding these factors is critical to implementing effective prevention strategies.
Global Trends in Cardiovascular Mortality
In high-income countries, cardiovascular mortality has declined significantly over the last 20 years. The World Health Organization’s (WHO) MONICA Project highlighted dramatic reductions in deaths from coronary heart disease and stroke across many populations. For example, in the United Kingdom, coronary heart disease mortality dropped by 42% between 1981 and 2000. Such improvements underscore the effectiveness of population-wide initiatives and healthcare interventions.
Primary Prevention Strategies
Primary prevention focuses on reducing the risk of developing CVDs. Lifestyle changes are at the forefront of this approach:
- Diet: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can lower cholesterol levels and blood pressure.
- Exercise: Regular physical activity strengthens the heart and improves circulation.
- Smoking Cessation: Quitting smoking significantly reduces the risk of CVDs within a few years.
- Public Health Initiatives: Campaigns promoting awareness of healthy habits have played a pivotal role in decreasing risk factors.
Secondary Prevention Strategies
Secondary prevention targets individuals who have already experienced cardiovascular events. Strategies include:
- Medical Interventions: Use of medications like aspirin, statins, and beta-blockers.
- Rehabilitation Programs: Tailored exercise and counseling sessions post-heart attack or stroke.
- Ongoing Monitoring: Regular health check-ups to detect and manage recurring risks.
Impact of Population-Wide Initiatives
Countries like Finland have demonstrated the power of population-wide initiatives. Comprehensive public health policies focusing on reducing smoking rates, improving diets, and promoting physical activity led to significant declines in CVD mortality. These initiatives highlight the importance of collective action in addressing public health challenges.
Role of Individual Healthcare Interventions
Healthcare systems have evolved to prioritize early detection and effective treatment of CVDs. Advances include:
- Medications: Statins and anticoagulants reduce cholesterol levels and prevent blood clots.
- Technological Innovations: Tools like wearable heart monitors and AI-driven diagnostic systems enhance early detection.
- Emergency Care: Improved ambulance services and acute care protocols have significantly increased survival rates after heart attacks and strokes.
Factors Driving Declining Mortality Rates
Key factors contributing to reduced mortality include:
- Enhanced healthcare delivery systems.
- Advances in treatment technologies.
- Public health campaigns that promote awareness and risk reduction.
Challenges in Low and Middle-Income Countries (LMICs)
Unlike high-income nations, LMICs face a growing burden of CVDs due to limited access to healthcare and prevention programs. Bridging the gap requires adapting successful strategies from high-income countries to local contexts.
Future Directions in Prevention
Innovations in cardiovascular health are paving the way for more effective prevention:
- Artificial Intelligence (AI): AI tools predict cardiovascular risks based on health data.
- Personalized Medicine: Genetic research tailors prevention strategies to individual profiles.
- Integrating Mental Health: Recognizing stress and depression as key risk factors for CVDs.
Recommendations for Individuals
To minimize the risk of heart attacks and strokes:
- Adopt Healthy Habits: Balanced nutrition, regular exercise, and stress management are vital.
- Recognize Warning Signs: Seek immediate medical attention for symptoms like chest pain or sudden weakness.
- Stay Proactive: Regular check-ups can detect risk factors early.

1. What are the main risk factors for heart attacks and strokes?
Risk factors include high blood pressure, high cholesterol, smoking, obesity, diabetes, and a sedentary lifestyle.
2. How can diet help prevent cardiovascular diseases?
A diet rich in fruits, vegetables, and whole grains reduces cholesterol and blood pressure, lowering the risk of CVDs.
3. What role do medications play in prevention?
Medications like statins and anticoagulants manage risk factors such as high cholesterol and prevent blood clots.
4. Why are mortality rates declining in high-income countries?
Declines are attributed to public health initiatives, medical advancements, and lifestyle changes.
5. What steps can individuals take to reduce their risk?
Lifestyle changes, regular check-ups, and adherence to prescribed medications are key.
6. How does mental health affect cardiovascular health?
Stress and depression can increase the risk of heart disease and strokes, making mental health management crucial.